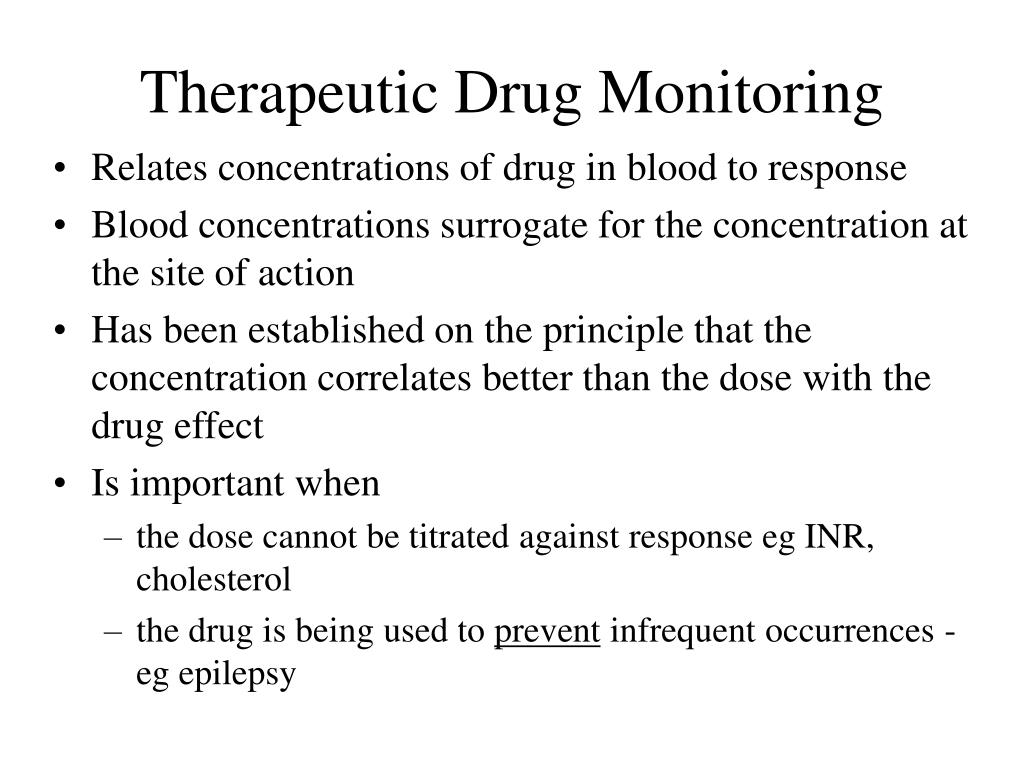
Therapeutic drug monitoring (TDM) is a medical practice that involves the careful measurement and analysis of medication levels in the body to optimize treatment and reduce the risk of adverse drug events. This is especially important for medications with a narrow therapeutic index, which means that they have a small range of effective doses that can be safely administered. By closely monitoring these medications, healthcare providers can ensure that patients are receiving the right amount of medication to effectively treat their condition without experiencing harmful side effects.
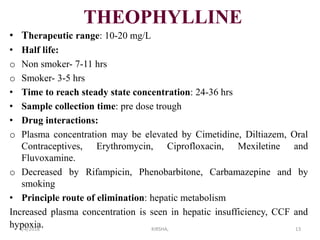
TDM is typically used for medications that are metabolized slowly or have a large inter-individual variation in their pharmacokinetics, such as antiepileptic drugs, immunosuppressants, and some psychiatric medications. It can also be used for patients who may be at risk of developing toxicity due to their age, sex, genetics, or other factors, or for patients who are taking multiple medications that may interact with each other.
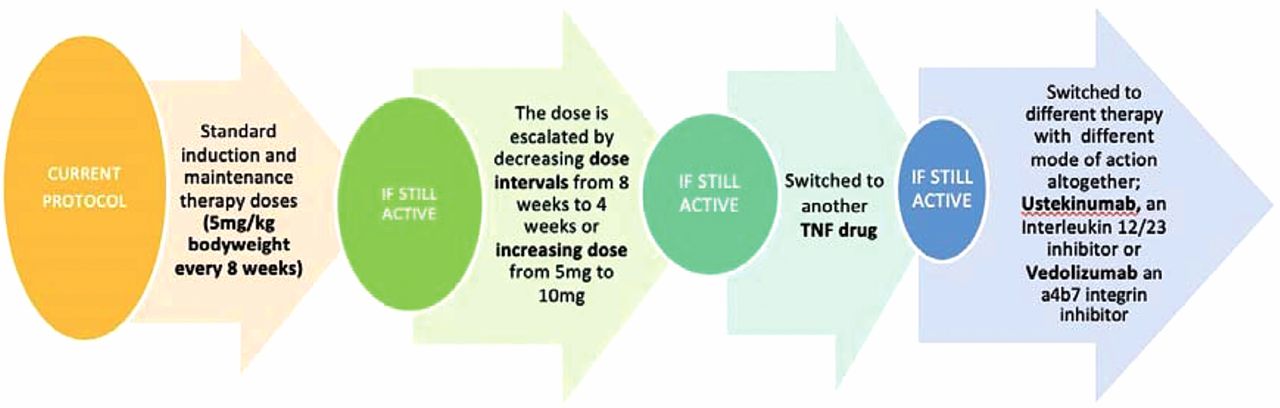
The process of TDM involves collecting blood samples from the patient at various intervals and analyzing them for the presence and concentration of the medication being monitored. These results are then compared to therapeutic reference ranges, which are established based on clinical studies and expert opinions, to determine whether the patient's medication levels are within the optimal range. If the levels are too low, the healthcare provider may adjust the dosage or frequency of the medication to ensure that the patient is receiving sufficient treatment. If the levels are too high, the provider may reduce the dosage or frequency to prevent toxicity.
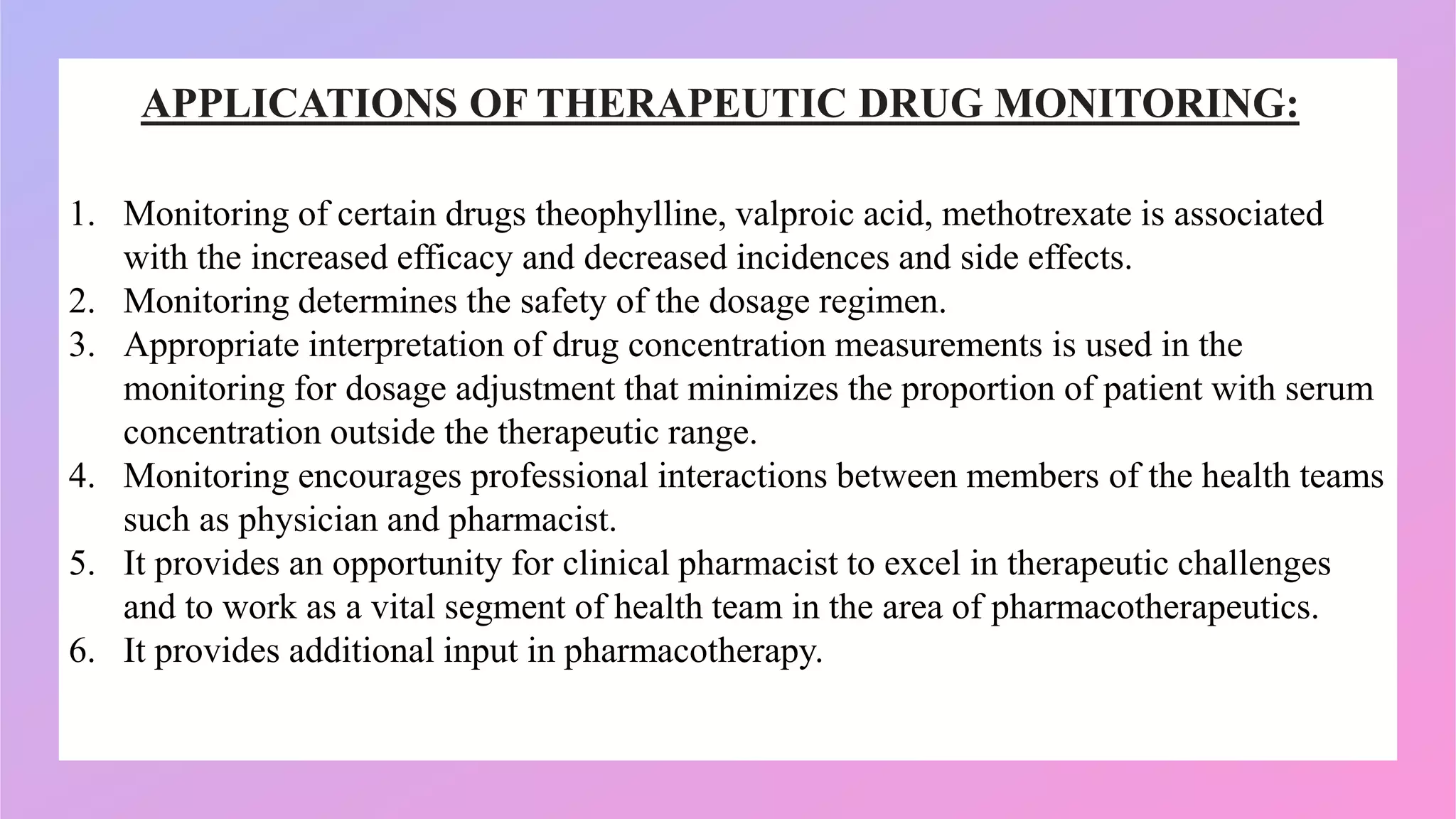
TDM can provide valuable insights into a patient's medication regimen and help optimize treatment outcomes. It can also help identify potential drug-drug interactions, inadequate absorption or metabolism, or non-compliance with the prescribed treatment. In addition, TDM can help healthcare providers detect and prevent adverse drug events, such as drug-induced liver injury, nephrotoxicity, and bone marrow suppression, which can have serious consequences for the patient.
There are several challenges to implementing TDM in clinical practice. One challenge is the cost and availability of specialized laboratory equipment and trained personnel needed to analyze the blood samples. Another challenge is the variability in the reference ranges used by different laboratories and the lack of standardization in the TDM process. Additionally, TDM requires close collaboration between the healthcare provider, the laboratory, and the patient, which may be difficult to achieve in a busy clinical setting.
Despite these challenges, TDM can be a valuable tool in the management of patients receiving medications with a narrow therapeutic index. By closely monitoring the levels of these medications in the body, healthcare providers can ensure that patients are receiving the right dosage to effectively treat their condition while minimizing the risk of adverse drug events.