The sacral plexus is a network of nerves located in the lower back region of the body, specifically in the pelvis. It is responsible for providing sensory and motor innervation to the lower extremities, including the legs, feet, and pelvic region.
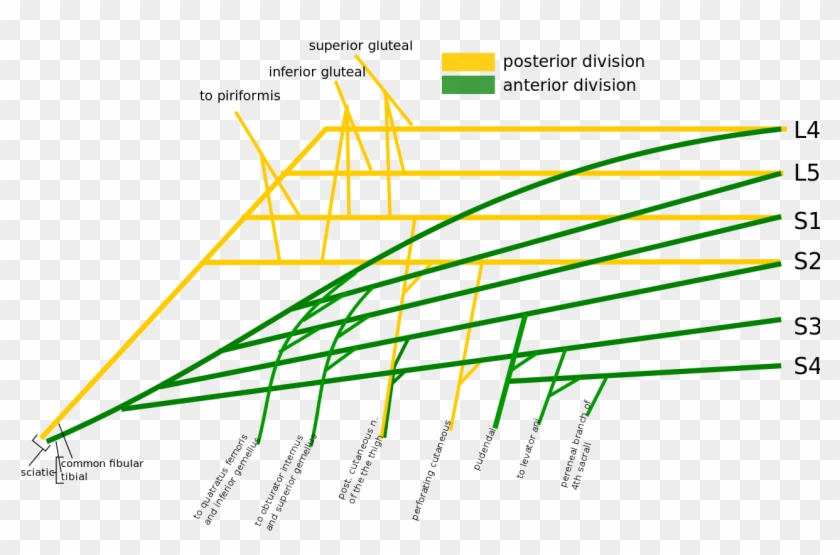
The sacral plexus is formed by the joining of several spinal nerves, including the L4, L5, S1, S2, and S3 nerves. These nerves originate from the lumbar and sacral regions of the spinal cord and then come together to form the sacral plexus. From here, the sacral plexus divides into several smaller nerves that travel to various parts of the lower extremities.
One important function of the sacral plexus is to provide sensory innervation to the skin of the lower extremities. This allows us to feel sensations such as touch, pressure, and temperature in our legs, feet, and pelvic region. The sacral plexus also plays a role in the sensation of pain and sexual arousal in these areas.
In addition to providing sensory innervation, the sacral plexus also plays a crucial role in the movement of the lower extremities. It supplies motor innervation to the muscles of the legs, feet, and pelvic region, allowing us to perform actions such as walking, running, and standing.
Damage to the sacral plexus can result in a range of problems, including sensory and motor deficits in the lower extremities. In severe cases, such damage can lead to paralysis of the legs and feet. Injuries to the sacral plexus can occur due to trauma, such as a car accident or a fall, or they can be the result of certain medical conditions, such as diabetes or spinal stenosis.
In conclusion, the sacral plexus is a crucial network of nerves that plays a vital role in the functioning of the lower extremities. It provides sensory and motor innervation to the legs, feet, and pelvic region, allowing us to feel sensations and move these parts of the body. Damage to the sacral plexus can result in a range of problems, including sensory and motor deficits and, in severe cases, paralysis.
MR Lumbar Sacral Plexus WO or WWO Neuro Protocol

The largest and only terminal branch is the sciatic nerve that provides two divisions:Â tibial nerve and common fibular peroneal nerve. J Brachial Plex Peripher Nerve Inj. This stands for Superior Gluteal, Inferior Gluteal, Sciatic, Posterior cutaneous nerve of thigh, Pudendal. A major drawback of this study is lack of clinical correlation of dose distribution in LSP and late toxicity. Indeed, Winnie postulated that, with firm compression immediately below the needle and a sufficient volume of local anesthetic, it is possible for the local anesthetic solution to diffuse toward the psoas muscle and consequently produce a block of the femoral, obturator, and lateral femoral cutaneous nerves. Neuropathy can also occur due to vitamin B12 deficiency, certain medications such as chemotherapeutic medications , toxins such as lead , alcohol, and metabolic illnesses.
Anatomy of the Lumbar and Sacral Plexus

There are five total nerve plexuses in the human body emerging from the spinal cord. Four nerves that come from the sacral region of the spinal cord S1, S2, S3, and S4 , form most of the sacral plexus. The axial slices of the planning CT scan of a representative patient at various levels are shown in Figure 1, and the lumbosacral plexus is digitally reconstructed, as shown in Figure 2. Although, the exact mechanism is not clear, it is thought to be associated with localized ischemia and subsequent soft-tissue fibrosis caused by microvascular insufficiency. This runs down into the pelvis to meet the sacral roots as they come out from the spinal cord. In all cases, the sciatic nerve is approached at the level of the lesser trochanter.
Sacral Plexus

In 50% of cases, this division occurs in the obturator groove, but it may also occur before or after the groove. The nerve enters the posterior The nerve has an anteroposterior and superoinferior range of cutaneous and fascial supply between the anterior and posterior axillary lines from the buttock to the middle of the calf muscles. From the surface downward, there is a subaponeurotic plane, containing lymphatics and vessels, followed by two aponeurotic planes: the fascia lata, stretching between the sartorius and adductor longus muscle, and the aponeurosis of the psoas major, iliacus, and pectineus muscles: the fascia iliaca. Its roots are from the S1, S2, and S3. It is located on the surface of the posterior pelvic wall, anterior to the piriformis muscle.
Sacral plexus Anatomy

Four nerves that come from the sacral region of the spinal cord S1, S2, S3, and S4 , form most of the sacral plexus. The recommended dose of gadolinium DTPA injection is 0. It provides motor innervation to the biceps femoris in the thigh, digitorum brevis in the foot, and all of the muscles in the anterior and lateral aspects of the leg. It hinders motor functions of the leg and foot. The sacral plexus begins as the anterior fibres of the spinal nerves S1, S2, S3, and S4.