Trauma radiography positioning refers to the specific positioning of a patient during the acquisition of radiographic images for the purpose of evaluating and diagnosing injuries sustained in a traumatic event. The importance of proper positioning in trauma radiography cannot be overstated, as it directly affects the quality of the images obtained and, subsequently, the accuracy of the diagnosis.
There are several factors that must be considered when positioning a patient for trauma radiography. The first and foremost consideration is the patient's comfort and safety. The patient may be in significant pain or may have suffered injuries that prevent them from being positioned in certain ways. It is important to minimize any additional discomfort or risk of further injury by carefully positioning the patient in a way that is both comfortable and safe.
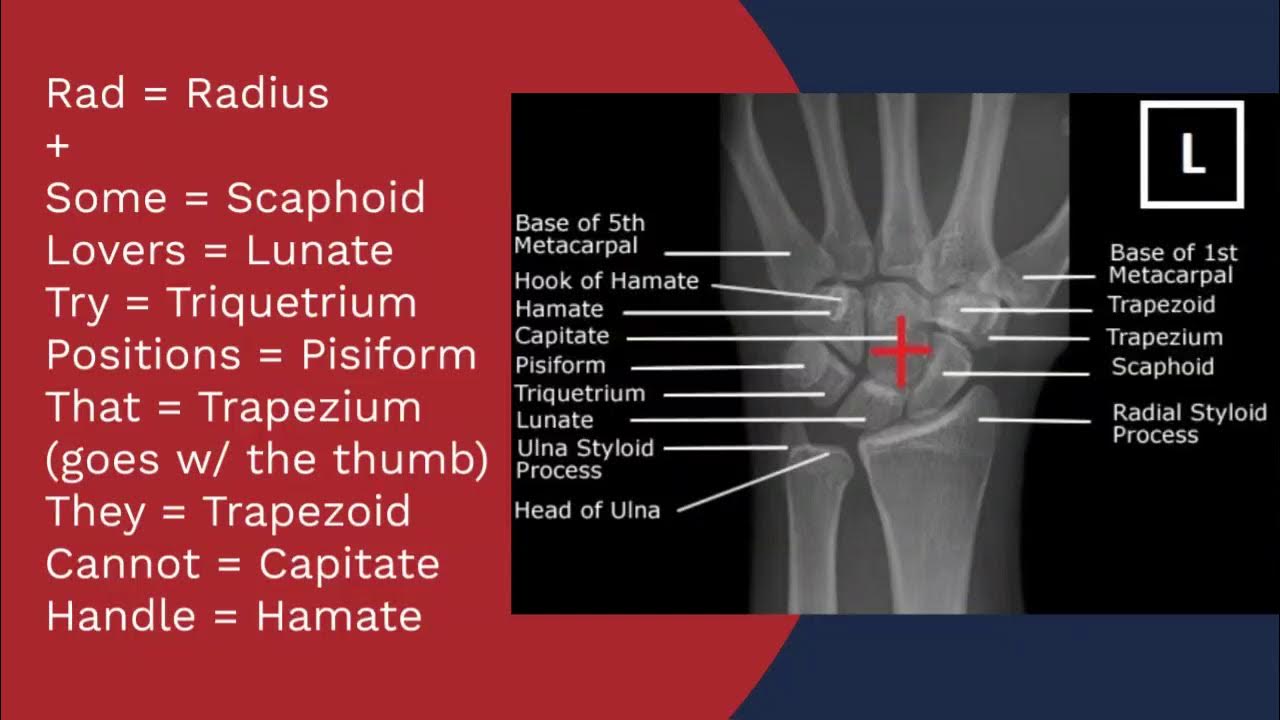
In addition to comfort and safety, the specific trauma being evaluated also plays a role in determining the appropriate positioning. For example, fractures of the lower extremities may require the patient to be positioned standing or sitting, while fractures of the upper extremities may require the patient to be positioned in a supine (lying on their back) or lateral (lying on their side) position.
Proper positioning also depends on the type of imaging modality being used. Different modalities, such as x-ray, computed tomography (CT), and magnetic resonance imaging (MRI), have specific positioning requirements in order to optimize image quality. For example, CT scanners require the patient to be positioned in a specific way in order to achieve the necessary spatial resolution and contrast.
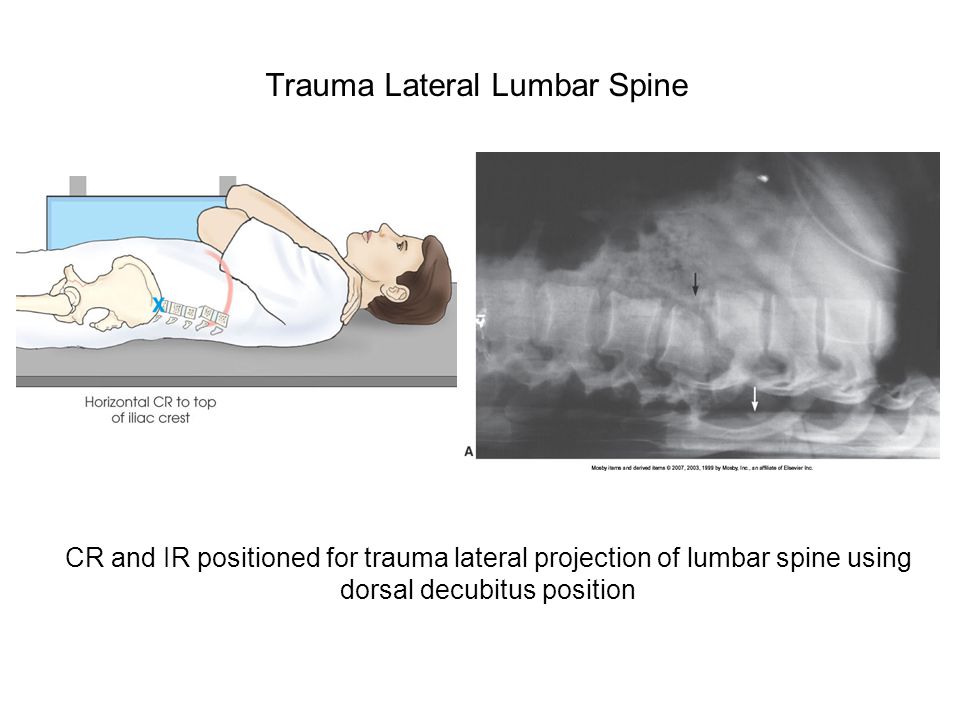
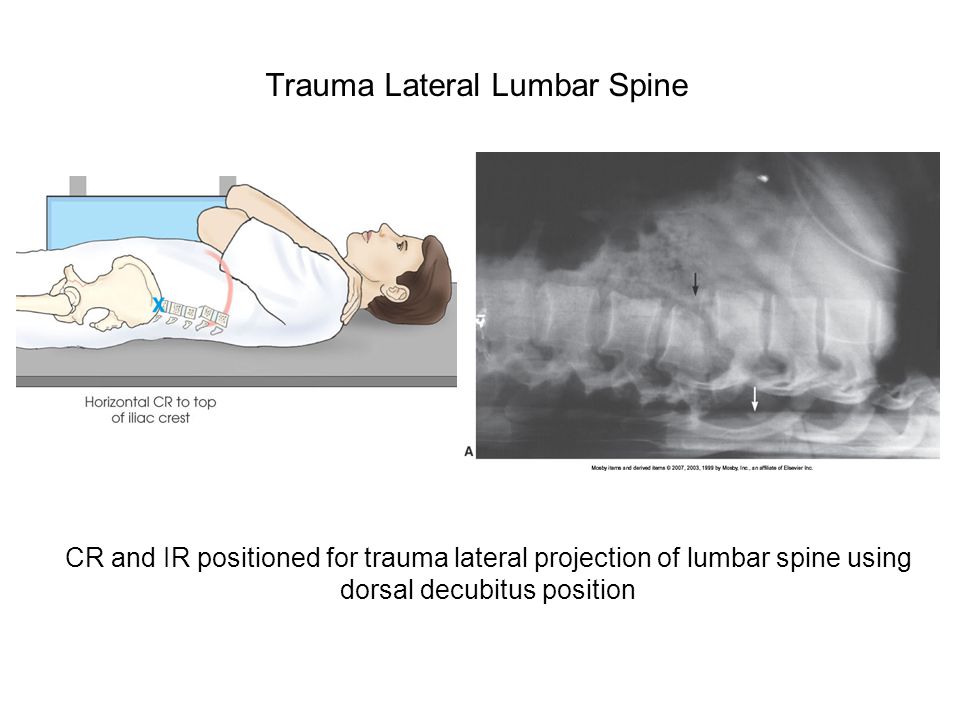
In addition to the patient's comfort and safety, the specific injury being evaluated, and the imaging modality being used, the positioning of the body part being imaged is also important. Proper positioning allows for optimal visualization of the injury and reduces the risk of superimposition, where structures overlap on the image, making it difficult to accurately interpret the image.
In summary, trauma radiography positioning is an important aspect of acquiring high-quality radiographic images for the purpose of evaluating and diagnosing injuries sustained in a traumatic event. Proper positioning considers the patient's comfort and safety, the specific injury being evaluated, the imaging modality being used, and the positioning of the body part being imaged.
TRAUMA RADIOGRAPHY

Trauma is the leading cause of death in the United States for persons of 1 to 34 years old. Penetrating trauma includes gunshot wounds GSWs , stab wounds, impalement injuries, and foreign body ingestion or aspiration. Obtaining lateral views generally requires penetrating a greater thickness of soft tissue, particularly in large patients, and often produces very limited quality images. In facilities where CT is not readily available for emergency patients, fractures of the pelvis may require a cystogram to determine the status of the urinary bladder. It has largely been supplanted by the FAST exam and is considered an optional skill in the current edition of ATLS.
Radiology: Imaging Trauma Patients in a Deployed Setting

Ensure to select the correct language at the time of scan setup for each patient. Professionalism: Ethical conduct and professionalism in all situations and with every person is a requirement of all health care professionals, but the conditions encountered in the ED can be particularly complicated. The patient may exhibit any combination of symptoms noted, and will have fruity-smelling breath. If patients requiring an xray of the chest. Quality - The quality of a radiograph does not have to sacrifice to produce an image quickly. Symptoms include diaphoresis, cool and clammy skin, decrease in venous pressure, decrease in urine output, thirst, and altered state of consciousness.
Trauma Radiography
This scope of practice for radiologic technicians varies from state to state and country by country. The brain has little healing power, so any injury to it must be considered potentially permanent and serious. Pelvic Fracture it has a high mortality rate of all open fractures and are as high as 50%. Imaging professionals are essential to the diagnosis of the injuries sustained during traumatic events, so extra study in this area of imaging is necessary. Trauma is defined as any physical damage to the body caused by a sudden, unexpected, dramatic, forceful, violent or accident event or fracture etc. Anticipation: Anticipating required special projections or diagnostic procedures for certain injuries makes the radiographer a vital part of the ED team. A central line can be used for contrast power injection.
Radiography Positioning Guide: Trauma Radiography

The radiographer should wear gloves, mask, eye shields, and gown when appropriate. During film processing, an eye contact with your patients is impossible, call for help. Physicians and many nurses specialize in trauma care. Alternatively in the setting of significant lower extremity trauma such as dismounted complex blast injury, the scan can be performed through the lower extremities default through the feet allowing evaluation of skeletal and vascular injury of the lower extremities. Level III centers are usually located in smaller communities where Level I or Level II care is unavailable.